Postpartum depression: A mini-review
DOI:
https://doi.org/10.5281/zenodo.7400409Keywords:
Anhedonia, depression, post-partum, stressAbstract
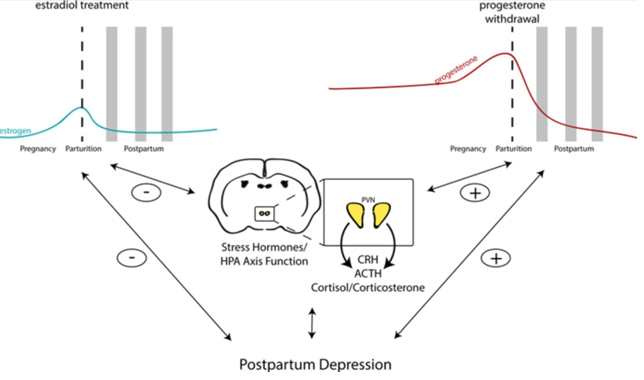
Stress and traumatic past experiences are two of the main risk factors for the development of postpartum depression. Reprogramming of the HPA axis and epigenetic alterations, which can also affect HPA function, are two neuroendocrine changes reported in postpartum depression that is linked to stress and negative life events. Because it is well established that stress hormones affect neuroinflammation, altered HPA axis function may have an impact on peripartum neuroimmune alterations that affect postpartum depression. On the other hand, neuroinflammation can affect how well the HPA axis functions, which may possibly be a factor in postpartum depression. By highlighting both clinical and fundamental science research findings, this review attempts to highlight the numerous potential pathophysiological pathways that contribute to postpartum depression. The discussion of postpartum depression risk factors may reveal information regarding potential neurological causes. The biology of postpartum depression is examined along with the evidence that suggests the involvement of neuroendocrine alterations, neuroinflammation, altered neurotransmitters, circuit malfunction, genetics, and epigenetics. This review emphasized neuroendocrine changes.
References
Epperson CN. Postpartum major depression: Detection and treatment. Am Fam Physician. 1999;59(8):2247–54.
Logsdon MC, Usui W. Psychosocial predictors of peripartum depression in diverse groups of women. Western Jrnl of Nurs Res. 2001;23(6):563–74.
Hay DF, Pawlby S, Angold A, Harold GT, Sharp D. Pathways to violence in the children of mothers who were depressed postpartum. Dev Psychol. 2003;39(6):1083-94.
Logsdon MC, Wisner KL, Pinto-Foltz MD. The impact of peripartum depression on mothering. J Obst, Gyn, and Neo Nurs. 2006;35(5):652–8.
Beck CT. The effects of peripartum depression on child development: A meta-analysis. Arch Psych Nursing. 1998;12(1):12–20.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of Gonadal Steroids in Women With a History of Postpartum Depression. Am J Psychiatry. 2000;157(6):924-30.
Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol. 2019;52:165-180.
Schiller CE, Meltzer-Brody S, Rubinow DR. The Role of Reproductive Hormones in Postpartum Depression. CNS Spectr. 2015;20(1):48-59.
Bloch M, Daly RC, Rubinow DR. Endocrine factors in the etiology of postpartum depression. Compr Psychiatry. 2003;44(3):234-46.
Pariante CM, and Lightman SL. The HPA axis in major depression: classical theories and new developments. Trends Neurosci. 2008;31(9):464-8.
Yim IS, Glynn LM, Dunkel-Schetter C, Hobel CJ, Chicz-DeMet A, Sandman CA. Risk of postpartum depressive symptoms with elevated corticotropin-releasing hormone in human pregnancy. Arch Gen Psychiatry. 2009;66(2):162-9.
Rich-Edwards J, Hacker M, Gillman M. Premature recommendation of corticotropin-releasing hormone as screen for postpartum depression. Arch Gen Psychiatry. 2009;66(8):917.
Meltzer-Brody S, Stuebe A, Dole N, Savitz D, Rubinow D, Thorp J. Elevated corticotropin releasing hormone (CRH) during pregnancy and risk of postpartum depression (PPD). J Clin Endocrinol Metab. 2011;96(1):E40-7.
Jolley SN, Elmore S, Barnard KE, Carr DB. Dysregulation of the hypothalamic-pituitary-adrenal axis in postpartum depression. Biol Res Nurs. 2007;8(3):210-22.
Bloch M, Rubinow DR, Schmidt PJ, Lotsikas A, Chrousos GP, Cizza G. Cortisol response to ovine corticotropin-releasing hormone in a model of pregnancy and parturition in euthymic women with and without a history of postpartum depression. J Clin Endocrinol Metab. 2005;90(2):695-9.
Murgatroyd CA, Nephew BC. Effects of early life social stress on maternal behavior and neuroendocrinology. Psychoneuroendocrinology. 2013;38(2):219-28.
Murgatroyd CA, Peña CJ, Podda G, Nestler EJ, Nephew BC. Early life social stress induced changes in depression and anxiety associated neural pathways which are correlated with impaired maternal care. Neuropeptides. 2015;52:103-11.
Carini LM, Murgatroyd CA, Nephew BC. Using chronic social stress to model postpartum depression in lactating rodents. J Vis Exp. 2013;(76):e50324.
Maguire J, Mody I. Behavioral Deficits in Juveniles Mediated by Maternal Stress Hormones in Mice. Neural Plast. 2016;2016:2762518.
Kara A. A review of childhood anxiety. J Clin Tri Exp Invest. 2022;1(3):64-70.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Unico's Review

This work is licensed under a Creative Commons Attribution 4.0 International License.